Why Is Fetal Shunting Performed?
In cases of abnormal fluid accumulation in the fetal cavities (bladder and chest) due to various pathologies, a catheter/shunt is inserted into the fetus in the womb to drain the excess fluid into the amniotic cavity. For this purpose, there are 2 applications:
- Vesicoamniotic shunt (between bladder and amniotic cavity):
It is used for ureteral obstruction such as bladder outlet stenosis. In posterior urethral valve (PUV), there is a narrowing or obstruction in the fetal urethra (at the lower end of the urinary tract), and urine backs up into the bladder, reducing the amount of amniotic fluid (oligohydramnios) and damaging the kidneys from the resulting pressure. If not intervened, the kidneys can be damaged and lose their function completely. In later stages, there is decreased/stopped lung development (pulmonary hypoplasia) and malformations of the face and extremities due to decreased amniotic fluid and pressure (Potter sequence). The vesicoamniotic shunt bypasses the pathologic site to provide an alternative route and maintain fluid levels by allowing urine to flow into the amniotic cavity. - Thoracoamniotic shunt (between the thoracic cavity and the amniotic cavity): Pathologic/abnormal fluids in the fetal thoracic cavity can lead to fluid accumulation in the pleura. As a result, proper development of the lungs in the thoracic cavity is reduced/stopped (pulmonary hypoplasia) and the newborn develops serious respiratory problems at birth. Unilateral or bilateral shunt applications may be required to shift this accumulation of fluid in the lungs to the amniotic cavity.
How Is Fetal Shunting Performed?
Ideally, the procedure should be performed before the lungs and kidneys of the fetus develop. For example, a detailed ultrasound is performed before the vesicoamniotic shunt, and urine samples are collected from the fetal bladder at 2-3 day intervals when screening for chromosomal abnormalities; if fetal renal function is still partially preserved, the procedure is initiated.
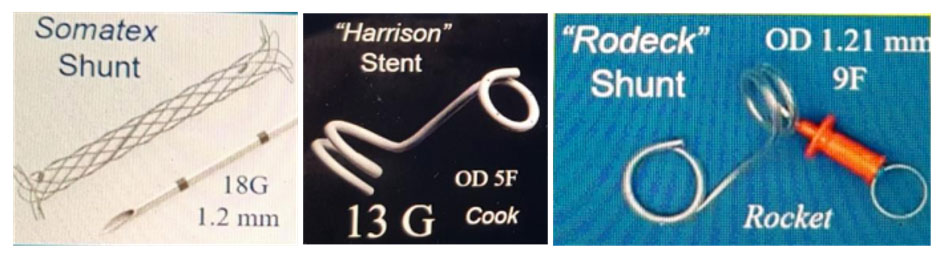
After antibiotics and local anesthesia are administered to the pregnant woman, a 3 mm diameter trocar needle and a metal cannula (tube) are inserted into the uterus and then into the fetal bladder under ultrasound guidance. After the trocar is removed, a drainage catheter is inserted into the cannula with one end of the catheter in the fetal bladder and the other end in the amniotic cavity. The position and function of the drainage catheter is confirmed by ultrasound. This catheter should remain in place and maintain urine flow until delivery. This procedure may also require an amnio-infusion, which delivers fluid to the amniotic sac.
What Can Happen After Fetal Shunting?
This procedure carries different risks for the expectant mother and the fetus. The expectant mother may experience bleeding, infection (peritonitis, chorioamnionitis), hemorrhage, or premature birth.
The shunt may not be successfully inserted into the bladder of the fetus, or even if inserted, it may be displaced by the movements of the fetus, or the kidney damage that has already occurred may not recover. In addition, depending on the procedure or underlying pathology, the fetus may die in the womb, be born prematurely and with low weight, or have respiratory or renal problems after birth.
The success rate is 25%, which means that even if the procedure is successful, it is not a perfect method. In other words, even after a successful procedure, there is a possibility of kidney failure after the baby is born.
On the other hand, thoracoamniotic shunt procedures are performed with a higher success rate and are more promising.


